Solving Bad Proximal Contact Problems in Posterior Composite Restorations.
Simon McDonald BDS MSc DDPH
As the inventor of the Triodent V3 Ring System, I am pleased to offer my thoughts on the various causes of poor proximal contacts in posterior composite restorations. Class II composite restorations are a common procedure in dental practice, and achieving proper proximal contact is critical for the long-term success of the restoration. Matrix placement plays a crucial role in achieving this proper contact, and dentists have several options, including sectional matrices and circumferential matrix bands. However, even with proper matrix placement, dentists may still face challenges in achieving proper proximal contact (Figure 1).
In this article, I will discuss the various factors that I believe contribute to poor proximal contact and the remedies for each of them.

Figure 1. Open contact between upper premolars.
It can be quite frustrating when a bad or open contact is unintentionally created. If ignored or left untreated, the problem will lead to food packing, secondary caries, halitosis and periodontal disease. This means that the contact point must be re-done immediately, often making the dentist run late. It also may reduce the confidence that the patient has in the dentist (Lisa Knowles, 2018).
Here are some of the reasons why I think dentists still get bad contacts (in order of importance):
- Tofflemire-type bands tend to pull away from the adjacent proximal tooth surface
- Un-contoured band leading to contact point too close to the marginal ridge
- Inadequate tooth separation
- Matrix retainer torques, rotates or twists matrix
- Undesirable tooth anatomy, position or large gap
- Narrow contact point when wider contact is desirable
- Matrix foil is too thick
The majority of matrices are either sectional or circumferential. In general, sectional matrices are easier to use on small restorations (Shaalan, 2020) but can be fiddly to place (Bailey, 2021) and are more likely to create marginal overhangs compared to circumferential bands (Loomans B. A., 2012), (Loomans B. A., 2009). On larger multi-surface restorations, sectional matrices can collapse inwards, especially when a separator ring is used (Figure 2). In contrast, circumferential matrices are less fiddly and work well for larger multi-surface restorations because they wrap around the tooth and create a better temporary “container”. Circumferential bands also can be tightened, create fewer overhangs (Loomans B. A., 2009), seal the margins and hold onto the tooth better than sectional matrices, especially when much of the tooth is missing*. However, tightening circumferential bands tend to pull the band inwards and away from the proximal surfaces of the adjacent teeth (Loomans, 2005) and are more likely to create open contacts. A recent survey (Shaalan, 2020) found that 44% of Egyptian dentists reported an open contact with circumferential bands. Tofflemire bands were used by 80% of these dentists.
I would now like to explore the reasons why Tofflemire-type bands cause these issues.
*[Not all patients can afford onlays or crowns.]
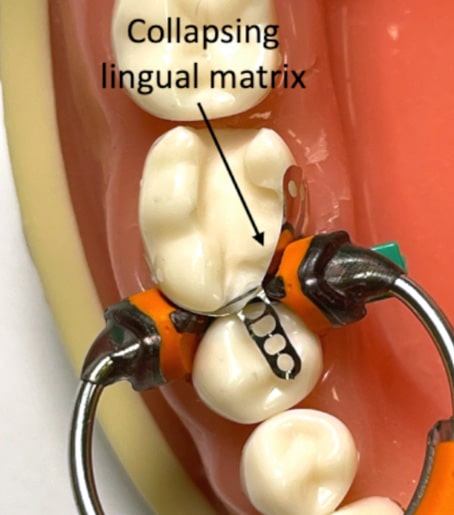
Figure 2. Sectional matrix collapsing into a large cavity.
Tofflemire-type bands tend to pull away from adjacent proximal tooth surfaces
How do we define poor contacts? Most dentists test their new restoration contact with dental floss and if they get a good “floss-click” they are happy and if not, they consider this is a bad contact.
On several occasions, I have placed a circumferential band, burnished well, wedged well and still got a bad contact. I have puzzled over this and struggled to identify the cause.
Although I have used dental floss for many years to confirm I have tight contacts, I did not know how thick dental floss was. So, I decided to measure it. I measured three common brands of floss with an accurate micro-meter and the floss thicknesses ranged from 60-90 microns. Most dental matrix bands are in the range of 35-45 microns, which is clearly around half the thickness of floss. The foil used to make modern matrices is remarkably thin and is thinner than human hair. After measuring the dental floss, a thought occurred to me: if a restoration was made with no tooth separation at all, the gap between the contacts should be the thickness of the matrix foil, which is 35 microns. Would I get a “floss-click” if the floss thickness is twice the gap thickness?
To test this, I placed a sectional matrix on a Typodont model that had a MO cavity and deliberately did not use any wedge or separating ring (Figure 3). I wanted to ensure that the matrix was actually touching the adjacent proximal tooth surface, so I tacked the tab to the adjacent tooth with flowable resin. I then filled the cavity, cured the composite, and removed the matrix. I now had a 35 micron gap and tried flossing and got a reasonable ‘floss-click” (Figure 4). I repeated the experiment with two matrices “spooned” together so that I created a 70 micron gap and the floss did not click.
There are two important conclusions that come from these simple, easy-to-repeat experiments:
1) if a poor contact does not produce a “floss-click” the gap must be greater than the matrix thickness and there must be an air gap between the matrix and the adjacent proximal tooth surface. In other words, the matrix must have pulled away from the adjacent tooth, unbeknown to the clinician.
2) that separation is not essential to get a ‘floss-click”.
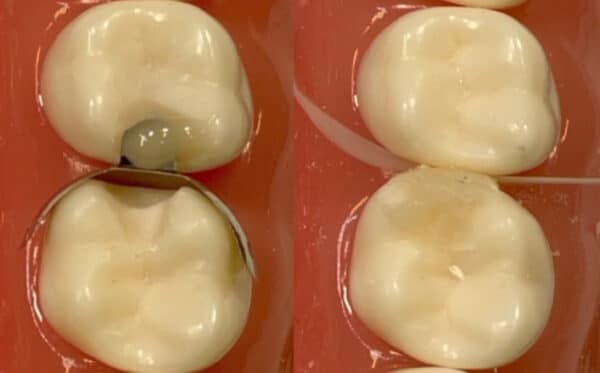
Figure 3. Shows a sectional matrix without a wedge or separating ring.
Figure 4. Shows a contact that was tight enough to give a “floss-click”.
Circumferential bands tend to pull the matrix inwards away from the adjacent teeth and clinicians have recommended pushing the matrix against the adjacent proximal surface with a hand instrument or a special instrument (Contact-Pro) while curing some flowable or regular composite that has been placed in the proximal box.
There are three problems with this technique:
- The hand instrument can become embedded in the flowable and be difficult to remove, potentially leading to fracturing of the composite in the box. This has happened to me and I had to remove all the composite and start over.
- There is evidence that this technique may increase overhangs(Loomans B. A., 2009).
- There is no composite at the contact point where the instrument was and this might allow the matrix to spring back, unbeknown to the clinician and leave an air gap, as described above.
- a narrower contact than desired can result as it is difficult to get a wide contact instrument into the proximal box, especially If the proximal box is small.
If we want to move something, there are only two choices: either push it or pull it. In contrast to the “pushing” technique described above, Rhondium has developed a novel “pulling” technique. The Tabbed version of the circumferential QuickConnect Anatomy Band has multi-holed “Tight-Contact-Tabs” on the top edge of the proximal sides of the band. These can be pulled with a probe while curing the composite (Figure 5 & 6). This idea overcomes all the issues listed above: no instrument to become embedded, the matrix cannot spring back and wide contacts can be achieved by pulling harder.
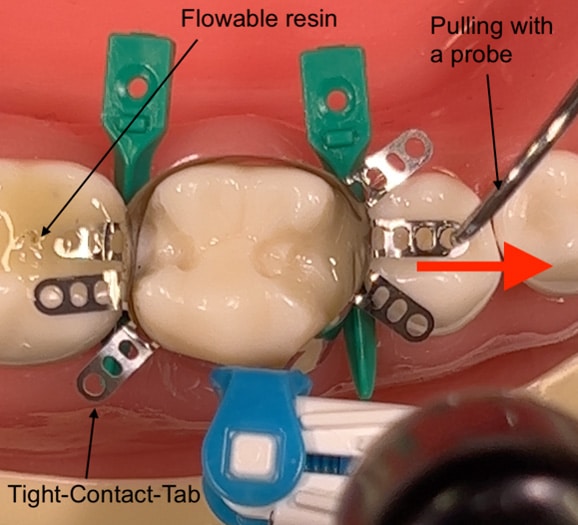
Figure 5. QuickConnect Anatomy Band
Additionally, one or more of the “Tight-Contact-Tabs” can be temporarily secured to the occlusal adjacent teeth with regular dental bond and a tad of flowable resin (no etch for obvious reasons!). This concept is utilized if the clinician is concerned that the matrix is pulling away from the adjacent tooth, a wide contact point is desired or if there is a large gap that needs closing. The temporary flowable resin can be removed with as sharp instrument such as a strong carver or No 12 scalpel.
This last technique allows both the mesial and the distal box to be simultaneously filled with composite and cured, saving valuable time (Figure 5). For example, only the tab on the distal side of the QuickConnect matrix could be secured with flowable and the mesial tab could be pulled with a probe while curing both proximal boxes or, for a more challenging case, both mesial and distal tabs could be tacked down.
When using sectional matrices, I recommend pulling on the tab of the matrix while curing as poor contacts can still occur with this type of matrix because the matrix may not actually be touching the adjacent tooth. See note below regarding wedges or separating rings pushing the adjacent tooth away from the matrix (Figure 8).
I now believe that the matrix pulling away from the adjacent tooth is the main cause of “unexpected” bad contacts. Prior to this, I had believed that it was caused by insufficient tooth separation or wedging. This new explanation led to the develop of the “Tight-Contact-Tabs” discussed above.
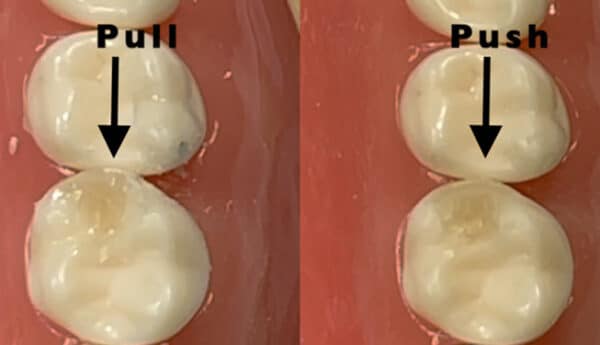
Figure 6. The image on the left shows a wider contact point created by pulling on the tab of the matrix and the image on the right shows the same cavity created using the push technique.
Un-contoured band leading to contact point too close to the marginal ridge
Un-contoured circumferential bands have a bad habit of creating “tin-can” restorations that have flat proximal contours (Figure 7).
Although some clinicians try to burnish un-contoured bands to overcome this problem, the amount of burnish required is guesswork and the springiness of the foil means that it can spring back, again, unbeknown to the clinician. Also, the burnishing can destroy the nice shape of pre-contoured bands.
The problem sometimes compounds when the occlusion is adjusted, as often an opposing cusp bites against the margin ridge of the new restoration. Minor occlusal adjustment can remove the contact point altogether because the only contact point is so close to the occlusal plane.
In my view, the solution is to avoid flat un-contoured circumferential bands and only purchase properly contoured circumferential bands that set the contact point at the anatomically correct height.

Figure 7. Shows an un-contoured matrix. (Bailey, 2021)
Inadequate tooth separation
It makes sense to separate teeth by at least the thickness of the matrix foil and this is in the region of 35-40 microns. In most cases, this can be achieved with a good wedge, especially if it is pushed in twice, with a few minutes periodontal relaxation time between each push. Although I invented one of the most popular separating rings (Triodent V3 Ring/ Palodent Plus Ring) I am now not convinced that rings are necessary for separation. They do function well to wrap the wings of the sectional matrix around the tooth. Note that the Triodent Wave-Wedges were not designed to separate but to help the apron of the matrix to follow the contours of the tooth close to the gingival margins.
Our in-house data found that “good old” wooden wedges generate more separating force that any separating ring we tested. One downside of some wooden wedges is that they can skewer the gingival papillae on the other side. Rhondium have designed a “Separator Wedge” that provides gradual and strong separating forces and has a “ski-jump” tip to prevent damage to the gingival papillae.
The use of separating wedges and separating rings can produce over-tight contacts. This rarely is a problem but patients can complain that their teeth “feel too tight”. This almost always resolves itself in a few days, by orthodontic-like micro-movements of the teeth.
I prefer to pre-wedge soon after the local anaesthetic has taken affect as this starts the tooth separation (Peña, 2016) and also the wedge protects the inter-proximal gingivae from damage during cavity-prep.
Unintuitively, tooth separation can potentially exacerbate the problem, because when you separate the teeth, the adjacent tooth’s contact point moves away from the matrix band thereby increasing the gap (Figure 8). Unless the matrix is pushed or pulled against the adjacent proximal tooth surface immediately prior to filling with composite, there is the potential that the benefit of tooth separation will be lost.
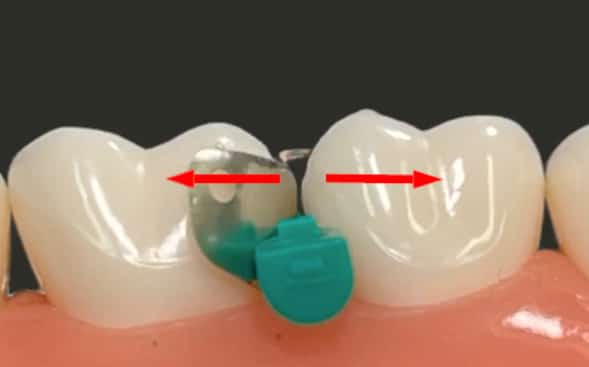
Figure 8. Shows how a wedge moves the adjacent proximal tooth surface away from the matrix.
Matrix retainer torques, rotates or twists matrix
The Tofflemire and the Siqveland retainers have both been available for many decades and most dentists know their deficiencies (Shaalan, 2020). The fundamental issues are caused by their weight, which causes torquing and twisting of the matrix band. This can contribute to the problems mentioned above where the band tends to pull away from the adjacent teeth. Another issue with these retainers is that the tightening part of the retainer protrudes forward and interferes with the patient’s lip or cheek, which can even cause the retainer and matrix to become dislodged.
There are several plastic “Tofflemire-like” retainers that are not heavy but the long handle can still interfere with the patient’s lip and cheek.
I believe that these types of retainers are best avoided unless cost is a major factor.
There are several circumferential bands on the market that are “retainerless”, meaning that the tightening tool detaches from the band. One of the earliest of these is the Automatrix by DentsplySirona. The Automatrix is not contoured, is 38 or 50 microns thick and the tightening tool tightens itself inside the coil of the matrix so that it cannot be released. The band must then be loosened to remove the tool, which increases the chances of creating ledges.
Another type of circumferential band was originally called the SuperMat by Kerr and later the Reel by Garrison in the USA. This matrix system is better than the AutoMatrix, in my opinion, but the reels can break if tightened too much and the tool has claws that grab the top edge of the reel and this can be tricky to re-engage and the claws can fail after a while. Both of these matrix tightening tools are expensive to replace (over US$500).
A more recent entrant to the market is the Palodent 360 by DentsplySirona. This has some nice features that include band contouring and it does not require any special tool because it is tightened by winding a “endo-file”-like knob. This is not a problem nearer the front of the mouth but further back it can be tricky placing one finger over the band to hold it in place while using a finger and thumb from the other hand to wind the knob. I’m not sure of the exact percentages but there many dentists who are resistant to placing their fingers in the back of the patient’s mouth.
The Rhondium QuickConnect Anatomy Band (Figure 9) has a fully detachable stainless-steel carrier that tightens the band using the same action as a Tofflemire, so it is easy to learn and use. The carrier is detached using a syringe-like motion to detach from the matrix. It is also easy to re-attach to adjust or remove by simply pushing the carrier back onto the matrix band capsule.
An additional benefit of the QuickConnect Anatomy Band is that it can be tightened firmly around the neck of the tooth while still flaring out toward the proximal contact points. This virtually eliminates unintentional ledges, seals the margins against crevicular fluid ingress and the matrix band remains in place even when there is little tooth to hang on to.

Figure 9. QuickConnect Anatomy Band from Rhondium
Undesirable tooth anatomy, position or large gap
Dentists frequently have to deal with non-ideal occlusions as many patients have unresolved or untreated orthodontic problems. Teeth can be rotated, tilted, out of the arch line and inter-proximal gaps can occur. Flexibility and ingenuity are required to solve these tricky cases. The Rhondium QuickConnect Anatomy band lends itself to these tricky cases as it has good contours and the tabs can be secured to close large inter-proximal gaps.
Narrow contact point when wider contact is desirable
Premolars tend to have narrow contact points while molars have broader contacts. As mentioned above, the “push the contact” method generally produces narrow contacts and it is difficult, if not impossible, to obtain broad contacts with this method, especially when the cavity is small. The tabbed version of the QuickConnect Anatomy Band enables a clinician to obtain broader contacts in two ways;
- Before curing, the tab that is in the best position is pulled towards the adjacent tooth while light-curing. The harder the tab is pulled, the broader the contact.
- If necessary, the tab can be temporarily bonded to the occlusal surface of the adjacent tooth. After applying bond and flowable, one of the tabs is pulled firmly while the flowable is cured. If this does not produce enough width, a second tab can also be secured in the same way and this produces a very satisfactory outcome.
Rhondium has a sectional matrix called the Sure Matrix that is fully contoured and has a longer tab with multiple holes that is ideal for the above two techniques.
Matrix foil is too thick
Matrix bands with a thickness of greater than 50 microns are available, particularly Mylar bands which are often 60 microns. This is not recommended as it can be difficult to separate the teeth enough to compensate for the band thickness.
Conclusion
The key to avoiding poor contact anatomy and tightness lies in selecting the best designed matrix bands and using the techniques covered above.
The most common unrecognised cause is that the matrix band pulls away from the adjacent proximal tooth surface without the clinician realising, as the matrices or separator rings obscure the inter-proximal space.
Contoured circumferential retainer-less matrix bands can provide many benefits for achieving proper proximal contact in large restorations and sectional matrices work well for small restorations. By using the appropriate technique and the best designed matrix bands, dentists can achieve successful and long-lasting restorations.
Conflicts of Interest
Dr Simon McDonald is a shareholder of the Rhondium company and joint inventor of the QuickConnect Anatomy Band.
References
Bailey, O. (2021, Nov). Sectional matrix solutions: the distorted trut. Retrieved from PubMed: https://pubmed.ncbi.nlm.nih.gov/34773017/
Lisa Knowles, D. (2018, July 19). Why contacts are so important to success in dentistry. Retrieved from Dentistry IQ: https://www.dentistryiq.com/dentistry/restorative-cosmetic-and-whitening/article/16367783/why-contacts-are-so-important-to-success-in-dentistry
Loomans. (2005, Sept 12). A randomized clinical trial on proximal contacts of posterior composites. Retrieved from https://pubmed.ncbi.nlm.nih.gov/16157438/
Loomans, B. A. (2009, Sep). Restoration techniques and marginal overhang in Class II composite resin restorations. Retrieved from PubMed: https://pubmed.ncbi.nlm.nih.gov/19524348/
Loomans, B. A. (2012, Jan). Proximal marginal overhang of composite restorations in relation to placement technique of separation rings. Retrieved from PubMed: https://pubmed.ncbi.nlm.nih.gov/21942287/
Peña, V. A. (2016, Jan). Sectional matrix: Step-by-step directions for their clinical use. Retrieved from PubMed: https://pubmed.ncbi.nlm.nih.gov/26768458/
Shaalan, O. O. (2020, Dec). Evaluation of Matrix Band Systems for Posterior Proximal Restorations among Egyptian Dentists: A Cross-Sectional Survey. Retrieved from PubMed: https://pubmed.ncbi.nlm.nih.gov/33642603/
