Innovative Dental Solutions
Rhondium develops restorative systems that make dentistry easier, faster, and more predictable. From matrix systems to separator rings, our products are engineered to deliver clinical precision and better patient outcomes.
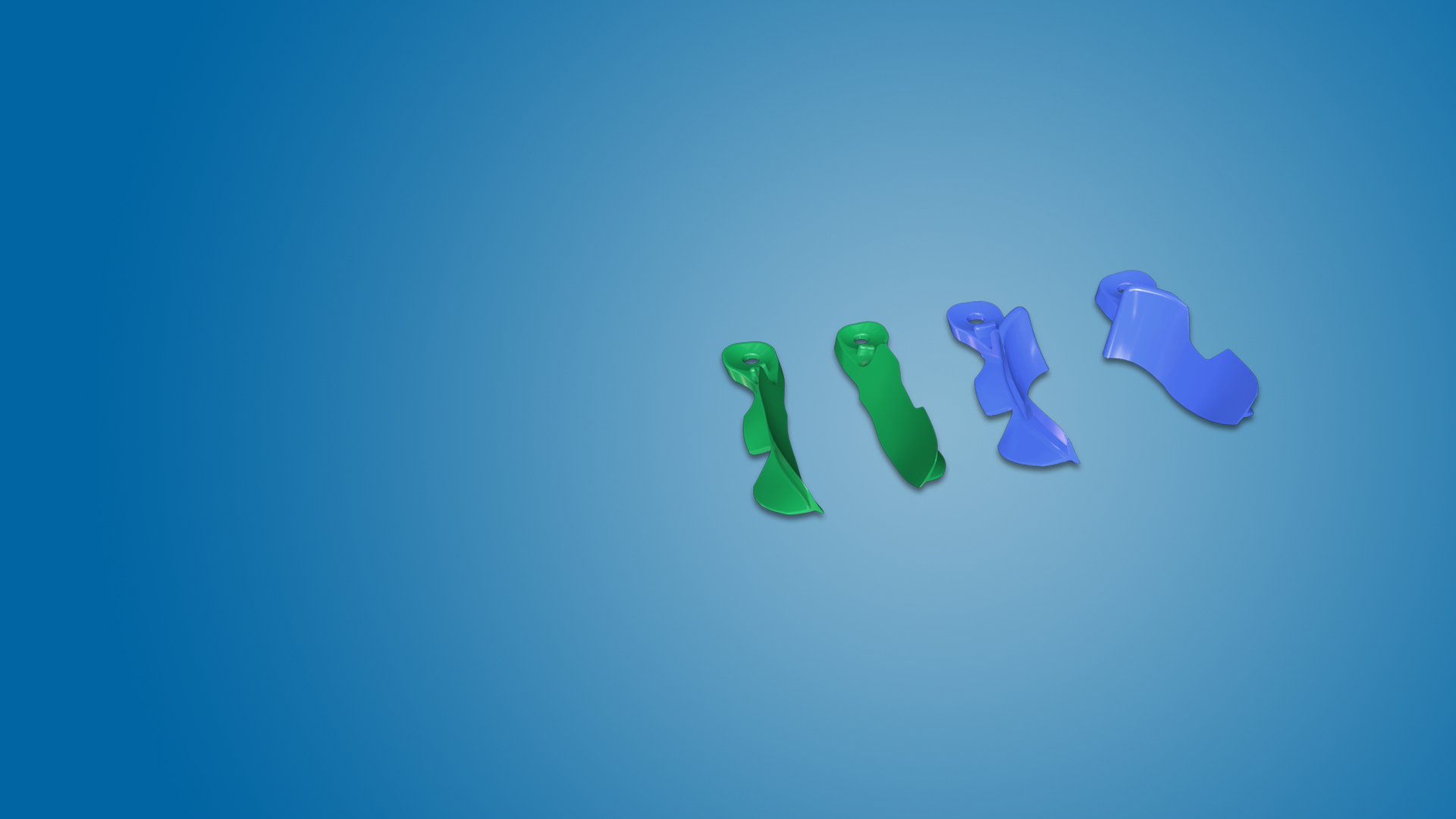
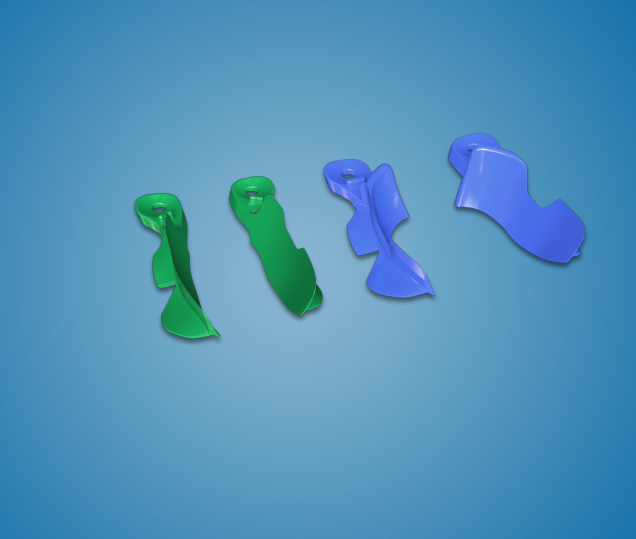
DME Wedge

The Deep Margin Elevation (DME) Wedge is one of Rhondium’s most popular products, trusted by dentists worldwide for its ability to deliver reliable results in challenging cases.
Its anatomically curved, asymmetric design follows the natural contours of the tooth, providing excellent contacts when cementing crowns or placing large restorations. By preventing gingival seepage, displacing the inter-proximal gingival col, and blocking out inter-proximal spaces, it ensures a clean, smooth tooth–cement–crown interface.
Often eliminating the need for a matrix band, the DME Wedge makes deep margin elevation simpler, more predictable, and more efficient.
Clinicians Thoughts
-
Dr Kirk HuffakerMountain View Endodontics
“Second time using this wedge and I gotta say...it came in clutch!! Made restoring this tooth so much easier and faster...
I'm kinda in awe actually...” -
Dr. Kate SmithThe Dental Lounge
These wedges isolate deep interproxal boxes like nothing I’ve seen before. They are brilliant for use in margin elevation techniques.
Shop DME Wedge
-
 Vendor:Rhondium Online Store
Vendor:Rhondium Online StoreDeep Margin Elevation Wedge Intro Pack
Regular price $69.00NZDRegular price -
 Vendor:Rhondium Online Store
Vendor:Rhondium Online StoreDeep Margin Elevation Wedge – Blue Large – 50 Pack
Regular price $105.00NZDRegular price -
 Vendor:Rhondium Online Store
Vendor:Rhondium Online StoreDeep Margin Elevation Wedge – Green Medium – 50 Pack
Regular price $105.00NZDRegular price -

 Vendor:Rhondium Online Store
Vendor:Rhondium Online StoreDeep Margin Elevation Wedge – Green & Blue – 100 Mixed Pack
Regular price $199.00NZDRegular price
-
Worldwide Shipping
Fast delivery within US, Australia & New Zealand.
-
Trusted by Dentists
Used daily in thousands of clinics worldwide.
-
Regulatory Approved
All products meet international dental standards.
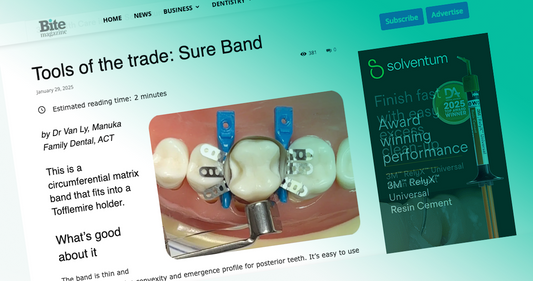
New M-RING

From the inventor of the world-renowned Triodent V3 Sectional Matrix System, the M-Ring delivers the dependable clinical results you expect from premium separator matrix rings - without the premium price tag.
Its patented ‘M’ shape offers the performance of a NiTi ring, engineered from medical-grade, autoclavable polymer.
The anatomically shaped, V-shaped tines ensure a secure grip and excellent matrix adaptation, while allowing wedge
placement without interference.
The M-Ring is proven to deliver consistent tension up to 100 cycles, setting a new benchmark for polymer ring durability.
It works equally well on premolars and molars, helping clinicians achieve consistent, reliable restorations every time.
Shop M-Rings
-

 Vendor:Rhondium Online Store
Vendor:Rhondium Online StoreM-Ring Sectional Matrix Intro Kit
Regular price $149.00NZDRegular price -

 Vendor:Rhondium Online Store
Vendor:Rhondium Online StoreM-Ring Sectional Matrix Kit
Regular price $229.00NZDRegular price -

 Vendor:Rhondium Online Store
Vendor:Rhondium Online StoreM-Ring - Single
Regular price $29.99NZDRegular price
What Dentists Say
-
 Dr John FlukeDental Products Editor
Dr John FlukeDental Products EditorDeliver your clinical best on every case
The QuickConnect Anatomy Band is an amazing system, you haven’t seen anything like this yet! If you are looking to deliver your clinical best on every case, with great contacts and amazing anatomical contours, you need to check this out.
-
 Dr Peter SidhomSmith Street Dental
Dr Peter SidhomSmith Street DentalI couldn’t work without it.
I have found the QuickConnect anatomy matrix system an extremely beneficial tool to have in my armamentarium. It fulfills a need that has been missing for a long time in the restoration of severely broken down teeth that required multiple stages to complete the restoration. Full composite crowns are much easier to achieve now. I couldn’t work without it.
-
 Dr Shayne ScottDental On Lawrence
Dr Shayne ScottDental On LawrenceStable, Secure, and Easy to Use.
I’m very happy with my QuickConnect kit. The bands and carrier snap together cleanly and separate without disturbing placement. They tighten securely, stay stable, and there’s no risk of pinching soft tissue. I regularly use the subgingival bands, and my go-to sizes are the 6.5mm bands for multi-surface posterior composites.