By Graeme Milicich BDS
Introduction
Mother Nature designed our teeth to primarily function in compression. They behave in a similar way to a masonry compression dome, like the Pantheon in Rome.1
Compression domes (Biodome) are structures that are designed into the enamel and range through several orders of magnitude from the macro down to the nano. When the Biodome is disrupted, the underlying dentin is then exposed to increased tension that increases with greater removal of critical areas of the Biodome, particularly the occlusal enamel.2,3,4
The most critical zones providing functional stability are associated with occlusal enamel. The more that can be retained, the more biomechanically stable the tooth remains in the long term.
Once the underlying dentin becomes exposed to tension, cracks can begin to propagate, eventually leading to failure that can present as teeth with lost cusps and/or pressure and temperature sensitivity due to cyclical flexing of the dentin as the crack propagates.
The Clinical Implications
When faced with cracked teeth and missing cusps, the restorative options can be quite complex.
Based on the concept of the compression dome and an understanding of force distributions, the ideal way to restore a badly damaged tooth is an adhesive ceramic onlay that retains as much of the cervical half of a tooth as possible. By keeping a restoration in the coronal half of the tooth, it is not exposed to radial hoop stress that occurs in the bottom half of a compression dome.5
When the option of placing a crown is discussed, the treatment the patient finally opts for is often tempered by patient economics.
Our restorative materials and teeth all cope best in compressive environments, so it makes sense to try and keep restorations out of areas exposed to significant tensile forces.1
In the emerging field of Biomimetic Dentistry, several techniques are being taught based on these principles of working with Mother Nature’s design.
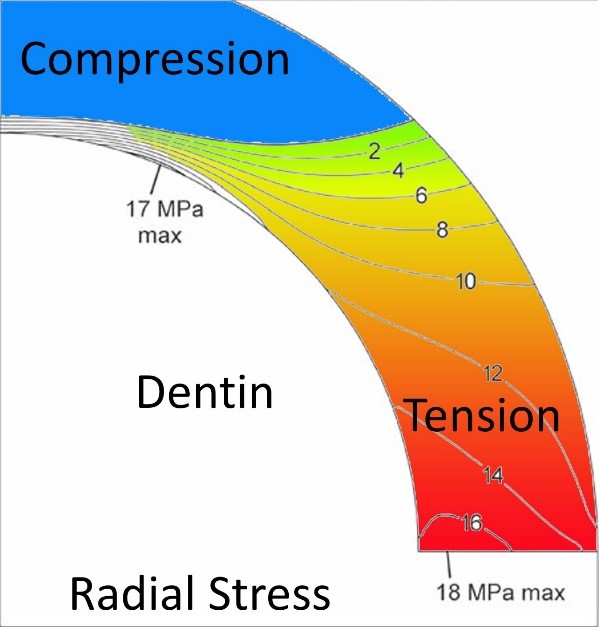
Figure 01: Increasing radial stress in the Bio-rim of the dental compression dome.5
New nomenclature is required to describe these functional zones on a tooth. The coronal half of the compression dome is being described as the Biodome, and the cervical half of the tooth that essentially supports the coronal compression dome is being called the Bio-Rim.
Ideally, restorations should avoid disrupting the Bio-Rim as much as possible, within the parameters dictated by existing damage from previous restorative efforts, trauma or decay. The goal is to avoid removing the Bio-Rim, which is what is required when placing a crown that is relying on cementation and the ferrule effect for retention. Retaining the Bio-Rim by placing adhesive onlay restorations helps to recreate the Bio-dome and restore biomechanical function.
The Basic Compression Dome Restoration Design
Adhesive ceramic onlays are effective at re-creating the compression dome and placing the underlying tooth structure back into compression.1
These restorations are so effective because they are bonded to the tooth with modern bonding systems that are now in the range of 40-50MPa of tensile strength, which is similar to Mother Nature’s tensile bond between enamel and dentin which has been measured at 45MPa.6
Clinically, dentists are faced with the conundrum that the best restorative option, an adhesive ceramic onlay, is often not a financially realistic one for the patient. As a consequence, the dentist is then faced with having to place a large direct adhesive restoration that is technically challenging.
The large volumes that can be involved create issues with maintaining a sound bond in an environment that can lead to high polymerization shrinkage stresses, if high C-Factor shrinkage stresses associated with mismanagement of increment size and placement are not addressed.
Unintentional voids between layers of composite are also a risk. Then there are the issues of creating predictably good contact points and recreating the occlusal morphology so the restoration looks like a real tooth.
The Biomimetic adhesive onlay, that primarily stays in the coronal half of the tooth, can be made from lithium disilicate, zirconia or one of the new hybrid composite systems.
Adhesive bonding is critical for compression dome restorations. Cementation techniques do not provide an adequate retentive tooth/restoration interface. All the material options are successful because they are all functioning in compression, avoiding the radial tensile forces present in the cervical Bio-Rim zone of the tooth.
These complex restorative systems are either lab generated or produced using in-house CAD/CAM. However, the dentist is often faced with the issue of cost for the patient, meaning the dentist is then forced to compromise and place a large direct restoration and face all the associated challenges.
A totally adaptable, lab generated onlay system, the OVC, that can be either placed as a direct, semi-direct or indirect restoration has been developed by Dr S McDonald (the inventor of the V3 Sectional Matrix System) at Rhondium that addresses all the problems associated with large direct restorations and takes no longer to place, while removing all of the direct restoration problems associated with contact points and occlusal anatomy.
When deciding on how to treat a badly damaged tooth, the dentist is often faced with the conundrum of what to do with a single remaining cusp, which may or may not be weakened, and struggle with the decision to overlay a cusp or not. If a crown had already been suggested, then all the cusps were going to be reduced anyway, so continuing to an onlay design instead is not problematic from this perspective.
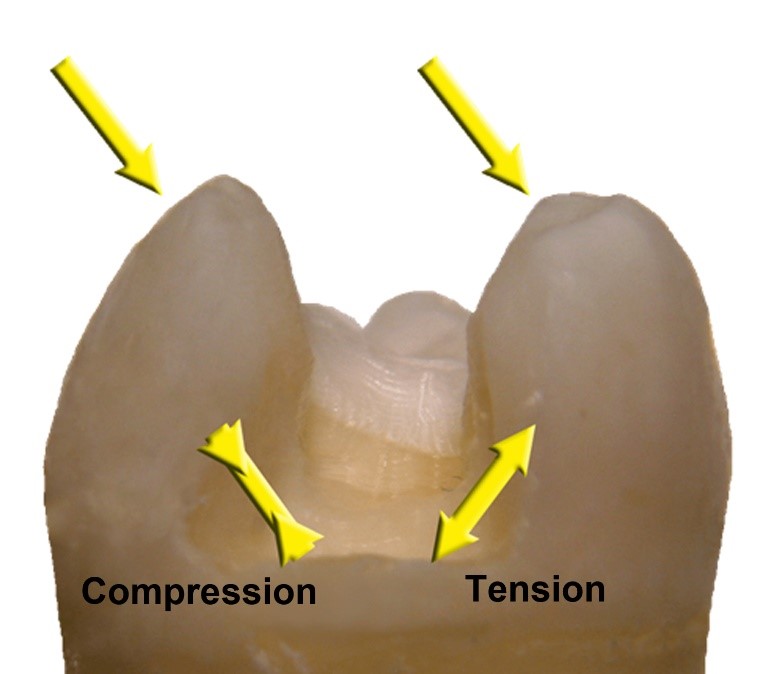
There is a simple guide as to whether a cusp should be overlaid or not. Ask the patient to chew on a piece of bite paper, to generate all the functional contacts on the tooth. If there are strong contacts on the occlusal planes of the cusp, the underlying dentin will be placed in tension, something that causes cracks to establish and propagate.
Looking to potential future failures, these cusps generally need protecting. If the occlusal load is on the buccal or palatal side of the cusps, the underlying dentin is in compression and these cusps tend to be functionally stable.
Figure 02: The left cusp is in compression, the underlying dentin is in compression and unlikely to develop a crack at the base. The load on the right cusp is placing the underlying dentin into tension and increases the probability of a crack developing over time.
If there is a cusp that should not be removed, and a custom adhesive CAD/CAM or lab generated is not an option for the patient, then the remaining option is a conventional direct composite. However, there are a significant number of teeth that truly benefit from the placement of an OVC, helping maintain the biomechanical integrity of the tooth by minimizing the reduction of the cervical half of the tooth.
Minimally invasive philosophies and techniques have to balance the desire to retain as much tooth structure as possible, with the need to design a restoration that has the best chance of longer-term success.
The OVC helps address the challenges of large direct restorations, while maintaining simplicity and predictability.
Failures in large direct restorations can be immediate. Open contacts, poor occlusal contour and anatomy, debonding induced post insertion sensitivity being the primary issues.
Once a fully bonded onlay solution is placed, be it lithium disilicate, zirconia or hybrid restorations, all function very effectively at the clinical level. Once bonded, the hybrid composite OVC performs at the same level as all the onlay techniques, with the huge advantage of being able to be placed in a single visit, no lab fees and no problems with temporization.
A Brief Summary of OVC
The technical simplicity of placing the OVC3 has been made possible due to several technical and material developments. Essentially, it is a strong, lab generated, heat-cured, highly processed zirconia hybrid composite occlusal onlay, with a layer of the same uncured hybrid
composite on the intaglio surface.
A plastic onlay replica helps guide the occlusal reduction required. Advanced wedging and separator systems combine with a revolutionary custom matrix system, that matches the onlay shapes, simplifying the placement and establishment of correct contacts and contours.
The system is very flexible, allowing for deep margin elevation techniques and if aesthetic demands are high, light-cured resin fissure staining can be placed.
Basic OVC Technique
The tooth is prepared, and the occlusal reduction is guided by the plastic replica.
If needed, any bio-base build-up or deep margin elevation can be performed at this stage and the prep remodified to ensure correct occlusal clearance. A contoured wedge system has been developed that assists in areas with deep interproximal margins.
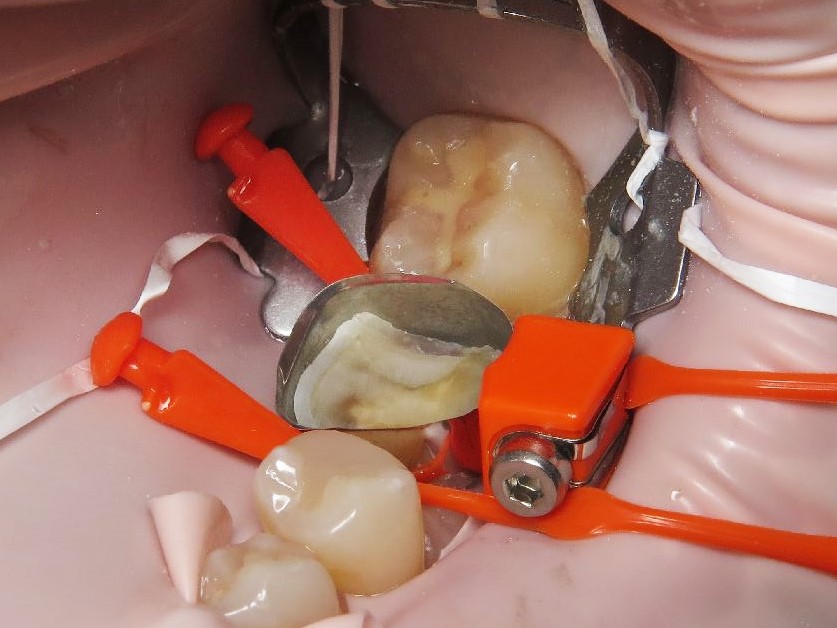
The McDonald Matrix Band is placed and wedged with either wooden wedges or Stretch-Wedges that have a separation force that exceeds that of the VRing System.
Following bonding of the tooth, the OVC is placed, aligning the marginal ridges with the adjacent teeth.
Excess unset composite is then removed and the restoration light cured.
Following removal of the matrix band, any excess composite on the buccal and lingual is contoured and polished.
The time taken ranges from ½ to 1 hour, depending on the complexity or need for any bio-base buildup or core fibre reinforcing that may be indicated.
Brief Case Study (courtesy Dr Venkat Canakapalli)
A patient presented with acute pulpitis associated with a deep distal cavity and undermined cusps with developing fractures.

Following endo, a fibre reinforced core was placed and a biobase built up to replace the lost dentin volume. The goal with a biobase is to reduce the potential space between the OVC onlay to about
1mm. This reduces the risk of composite shrinkage leading to a dentin debond.
The matrix placement is aided by the use of the Stretch Wedges, which also proved a separation force double that of the VRing system.
The matrix is thin, allowing it to be burnished out, combining with the strong separation of the Stretch Wedges (or wooden wedges) to create predictable contacts.
Figure 04.
The OVC is then placed, excess material removed, cured, then final contouring and polishing.
Figure 05.
If you have any questions for Dr Milicich about this article, leave a comment below.
References:
- Milicich G. The Compression Dome Concept: the Restorative Implications. Academy of Gen Dent Sept/Oct 2017. Pp 55-60.
- Rainey JT. A sub-occlusal transverse ridge: identification of a previously unreported tooth structure: the Rainey ridge. J Clin Pediatr Dent. 1996;21(1):9-13.
- 2. Rainey JT. The maxillary molar mesial-sub occlusal enamel web: identification of a previously unreported tooth structure: the maxillary Rainey web. J Clin Pediatr Dent. 1998;22(3):195-198.
21. Magne P, Oganesyan T. CT scan-based finite element analysis of premolar cuspal deflection following operative procedures. Int J Periodontics Restorative Dent. 2009;29(4):361-369. - Milicich G, Rainey JT. Clinical Presentation of Stress Distribution in Teeth and the Significance in Operative Dentistry. Pract Periodont Aesthet Dent 2000;12(7):695-700
- Chris Ford, Mark B. Bush, Brian Lawn. Effect of wear on stress distributions and potential fracture in teeth. Journal of Materials Science: Materials in Medicine, November 2009, Volume 20, Issue 11, pp 2243-2247
- Isao Urabe, Masatoshi Nakajima, Junji Tagami. Physical Properties of the Dentin-Enamel Junction Region. AmJDent 2000; 13:129 [intro2]